1. Background:
2. Why cardiac MRI is beneficial
Cardiac MRI is well suited for the examination of PDA because it can accurately quantify and locate the shunt, and the effect of the shunt on cardiac structure and function. It is totally non-invasive and uses gadolinium contrast.
3. MRI technique:
Short and long axis SSFP images are obtained to quantify LV volumes and LV systolic function.
Phase-contrast images are obtained perpendicular to the aorta just distal to the aortic valve, and pulmonary artery just distal to the pulmonic valve. For accurate results, an identically prescribed phase-contrast image of a stationary phantom is used for baseline correction of the flow data.
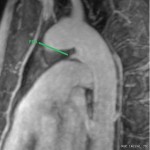
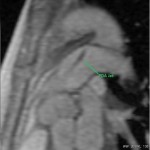
3D images of the aorta are obtained after contrast administration to visualize PDA.
4. Analysis:
PDA is unique in that it is the only shunt type that gives a Qp/Qs <1, when pulmonary blood flow is increased. This is an artifact where on typically quantifies Qp and Qs with MRI. Qp is typically measured in the main pulmonary artery just distal to the pulmonic valve, which is proximal to the site where the PDA inserts into the main pulmonary artery. As a result, Qp does not reflect the additional pulmonary blood flow that comes from the aorta. However, Qs .
The best way to determine the shunt volume is by calculating Qp/Qs using the aortic (Qs) and pulmonary artery (Qp) flows.
5. Which imaging findings affect treatment?
The severity of PDA can be quantified in terms of Qp/Qs. Surgery is generally reserved for patients with Qp/Qs > 1.5, unless they are going for cardiac surgery for other reasons.
6. Drawbacks of existing tests:
Echocardiography with color flow Doppler imaging is most commonly used to assess PDA.